Practice Policies & Patient Information
Welcome to Rea Valley Health Partnership
The doctors and staff at The Kings Norton Surgery, Ash Tree and Keynell Covert Surgery in Birmingham are proud to offer the highest standard of patient-centred healthcare.
Access to Records
In accordance with the Data Protection Act 1998 and Access to Health Records Act, patients may request to see their medical records. Such requests should be made through the practice manager and may be subject to an administration charge.
No information will be released without the patient consent unless we are legally obliged to do so.
Complaints
We always try to provide the best service possible but on occasions there may be the necessity to express a complaint. The following explains how this can be done so that any problems can be dealt with as quickly and efficiently as possible by our staff.
Making a complaint
Please put any complaint in writing to the Practice Manager. The Practice Manager will then carry out an investigation. You will be kept informed and given time scales for responses.
We have a duty of confidentiality to our patients and will act in strictest confidence. A patient’s consent must be obtained if it is not the patient making the complaint directly.
Dealing with the complaint
The Practice Manager can directly deal with administrative complaints whilst the Senior Partner will investigate clinical complaints.
You will receive a written acknowledgement of receipt of the complaint within five working days.
When the complaint is being dealt with it may be necessary for more information to be obtained by the person investigating and you will be contacted within 7 working days. In this case you may choose to discuss the matter by letter or telephone or in person (bringing a friend with you if you prefer) at a pre-arranged appointment.
You will receive a written response, usually within 10 working days.
By this stage we hope the problem has been resolved. However, if this is not the case we will try to suggest other avenues of approach to solve the problem.
You may not wish to raise your complaint with the practice, should this be the case you may contact the Parliamentary & Health Service Ombudsman to request a review of your complaint. Further help and advice is available from the Ombudsman’s Helpline on 0345 015 4033 (open 8:30 to 5:30 Monday to Friday) or by accessing their website (www.ombudsman.org.uk)
We are always prepared to listen to your concerns and will work with you to resolve these in a professional and conscientious manner. We would encourage anyone who is not entirely satisfied with their experience at the practice to contact a member of staff as soon as possible so that we may do everything we can to address any issues.
Confidentiality & Medical Records
The practice complies with data protection, GDPR and access to medical records legislation. Identifiable information about you will be shared with others in the following circumstances:
- To provide further medical treatment for you e.g. from district nurses and hospital services.
- To help you get other services e.g. from the social work department. This requires your consent.
- When we have a duty to others e.g. in child protection cases.
- Anonymised patient information will also be used at local and national level to help the Health Board and Government plan services e.g. for diabetic care.
If you do not wish anonymous information about you to be used in such a way, please let us know.
Reception and administration staff require access to your medical records in order to do their jobs. These members of staff are bound by the same rules of confidentiality as the medical staff.
Fair Use Policy
The following fair use policy has been designed by your practice team to support fair use and access of the online consultation platform and other practice resources.
Please read this carefully and contact your practice team if you have any queries.
We are committed to ensuring equitable access to our practice team to deliver the best possible service we can for you.
To ensure this, we ask all patients to contact our clinicians and admin staff in a fair, consistent and timely manner.
To help us and all patients at the surgery, we would like to kindly remind you that patients should use our online consultation platform, telephone access and other appointments in accordance with this Fair Use Policy.
Inconsiderate or unfair use of our resources may mean that another patient who wants to access their GP or other healthcare professional is unable to do so due to limited availability.
Examples of unfair use of our online consultation platform/telephone access/appointment usage may include, but are not limited to:
- Significant deviation from average use of the GP surgery e.g. submitting unreasonable numbers of online consultations
- Any form of abuse or harassment of our staff
If unfair use of the online consultation platform/telephone access/appointment usage significantly impacts our ability to deliver safe care to all patients, we reserve the right to review individual access to these resources. This process will include a series of communications with you followed by potential action.
Where a patient’s behaviour falls outside of that which is normally considered reasonable (e.g. breaches the NHS Zero Tolerance Policy) and leads to an irretrievable breakdown of the doctor-patient relationship, in a minority of cases this may also lead to the consideration of removal from the practice list itself.
Our commitment to you
- We will treat all patients equally with dignity and respect, without exclusion.
- We aim to provide a personal, friendly and confidential service to our patients.
- We aim to keep patients informed of our services, their rights and any other information which directly affects health treatment.
- We will offer access to our services in line with the patients’ assessed need.
- We will monitor and improve our systems to ensure we operate as efficiently as possible within the resources available to us.
- We operate a practice complaints procedure which may be used in confidence
- We welcome and consider all feedback from our patients.
Help us to help you
- Please only submit one online consultation for the issue you require help with but include as much information as possible in your request – submitting the same request repeatedly or chasing an answer within a short time frame will not necessarily result in a faster response.
- Keep appointments made with us or cancel in plenty of time.
- Bear with us if there is a delay – this may be due to another patient needing additional time or an emergency. We will try and keep you informed of anticipated delays.
- Use our service responsibly and do not expect immediate treatment for non-urgent / routine conditions.
- Consider other avenues of help for minor conditions – self-care, pharmacy, NHS111 etc. where appropriate.
- Utilise the services of other professionals in the practice – the GP is not necessarily always the most appropriate person to see.
- Allow sufficient time for processing of repeat prescription requests and please do not pressure staff to process sooner than the standard 48-hour time line
- Keep us informed of any name, address and telephone number changes.
- Treat us with respect. We will not tolerate verbal or physical abuse.
- Only request a home visit if you are too ill or physically incapable of attending the surgery. Your request will be triaged by telephone before a visit is carried out. A home visit may not be deemed to be appropriate.
Irretrievable breakdown of the doctor -patient relationship
Occasionally, patients may persistently act inconsiderately and their behaviour may fall outside of that which is normally considered to be reasonable. In such circumstances there may be a complete breakdown in the doctor-patient relationship.
If this situation occurs, we will take the following steps:
Steps we will take with the patient
- Inform the patient, either personally or in writing, that there is a problem.
- Explain the nature of the problem to the patient.
- Obtain the patient’s perspective and interpretation of the situation.
- Agree a contract of reasonable access with the patient if necessary.
- Monitor the situation and if further breeches occur consider this a breakdown in the practice-patient relationship. If this situation does arise, the process for the patient registering elsewhere will be commenced.
Steps we will take within the Practice
- Inform all appropriate members of the practice about the problem.
- The patient and possible reasons for the patient’s behaviour (e.g. disagreeableness, cultural differences, mental illness, personality disorder) will be discussed at a Practice Meeting.
Steps we will take if discussion fails to resolve the problem
- Inform the Patient Registration Department at Primary Care support england in writing of the practice decision to remove the patient and the reason why.
- Where appropriate, inform the patient in writing of the decision and the reason for removal from the list.
- Explain to the patient that he or she will not be left without a GP.
- Give the patient information on how to begin the process of registering with another practice and the expected timeline.
Fear of flying Kings Norton Surgery Policy
Benzodiazepine prescribing for flying, hospital/dental procedures or scans
Following review of the available guidance, the practice has taken the decision to stop prescribing benzodiazepine medications e.g. diazepam/lorazepam for fear of flying.This policy also covers requests for dental/hospital procedures or scans.
The reasons are for this as follows:
- Diazepam is a sedative, which means it makes you sleepy and more relaxed. If there is an emergency during the flight it may impair your ability to concentrate, follow instructions and react to the situation. This could have serious safety consequences for you and those around you.
- Sedative drugs can make you fall asleep, however when you do sleep it is an unnatural non-REM sleep. This means you won’t move around as much as during natural sleep. This can cause you to be at increased risk of developing a blood clot (DVT) in the leg or even the lung. Blood clots are very dangerous and can even prove fatal. This risk is even greater if your flight is greater than four hours.
- Whilst most people find benzodiazepines like diazepam sedating, a small number have paradoxical agitation and in aggression. They can also cause disinhibition and lead you to behave in a way that you would not normally. This could impact on your safety as well as that of other passengers and could also get you into trouble with the law.
- According to the prescribing guidelines doctors follow (BNF) Benzodiazepines are contraindicated (not allowed) in phobia. Your doctor is taking a significant legal risk by prescribing against these guidelines. They are only licensed short term for a crisis in generalised anxiety. If this is the case, you should be getting proper care and support for your mental health and not going on a flight.
- Diazepam and similar drugs are illegal in a number of countries. They may be confiscated or you may find yourself in trouble with the law.
- Diazepam stays in your system for quite a while. If your job requires you to submit to random drug testing you may fail this having taken diazepam.
- The sedating effects have the possibility of causing some respiratory depression, resulting in a drop in your oxygen level. Normal oxygen levels for a healthy person at 8000ft are around 90%, so with the 2 effects added together, this may become life threatening.
- NICE guidelines suggest that medication should not be used for mild & self limiting mental health disorders; in more significant anxiety related states – benzodiazepines, sedating antihistamines or antipsychotics should not be prescribed; Benzodiazepines are only advised for the short term use for a crisis in generalised anxiety disorder, i.e. acute anxiety emergencies & if this is the case, they would not be fit to fly anyway (potential risk to being able to allow completion of the flight without diversion) & fear of flying in isolation is not generalised anxiety disorder.
We appreciate that fear of flying is very real and very frightening. A much better approach is to tackle this properly with a Fear of Flying course run by the airlines. We have listed a number of these below.
Easy Jet
- fearlessflyer.easyjet.com
- Tel—0203 8131644
British Airways
- flyingwithconfidence.com/venues/manchester
- Tel—01252 793250
Virgin
- https://flywith.virginatlantic.com/gb/en/wellbeing-and-health/flying-without-fear.html
- Tel—01423 714900/1252250
With regards dental/hospital procedures or hospital scans, as per GMC guidance the responsibility for prescribing lies with the clinician arranging the scan/procedure. Please contact the requesting doctor/dentist to prescribe the benzodiazepine if they feel this is appropriate.
Freedom of Information
Information about the General Practitioners and the practice required for disclosure under this act can be made available to the public.
All requests for such information should be made to the practice manager.
General Data Protection Regulation
Please see our website privacy statement.
GP Net Earnings
All GP Practices are required to declare the mean earnings (i.e. average pay) for GP’s working to deliver NHS services to patients at each practice.
The average pay for GP’s working in Kings Norton Surgery in the last financial year was £98,775 before tax and National Insurance. This is for 1 full time GP, 7 part time GP’s and 0 locum GP’s who worked in the practice for longer than six months.
Mounjaro prescribing in General Practice
Soon GPs will be able to start prescribing Mounjaro for patients for weight loss in very specific patients.
NHS England has calculated this to be 220,000 patients across primary care and weight management services in hospital. This means that across our practice of 16,000 patients, approximately 30-40 patients will qualify for weight loss injections and some may already be using it.
We respectfully ask that due to limited resources in general practice, please avoid contacting the practice to ask for Mounjaro if you do not qualify for the injections. Sadly on the NHS, we are unable to help or prescribe this for you.
The cohorts and dates that people will be eligible are as follows:
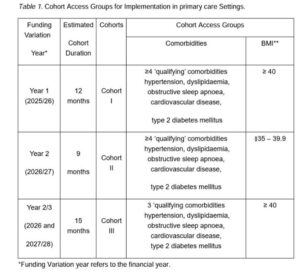
From end of June 2025 (cohort 1), to be able to be able to have Mounjaro prescribed by your GP, you will need a BMI of over 40 with the four of the five following conditions:
- Diagnosed hypertension
- Diagnosed sleep apnoea
- Diagnosed type 2 diabetes
- Diagnosed cardiovascular disease
- Diagnosed hypercholesterolaemia.
If you do not meet this criteria, we cannot prescribe for you (based on the current guidance).
We appreciate your support in this matter.
Non-NHS Third Party Prescribing Policy
Patient Charter
When and how can you contact your general practice?
Your general practice is open from 8.00am to 6.30pm, Monday to Friday.
Throughout these hours you, or your carer on your behalf, can:
- Visit the practice
- Call them
- Go online using the practice’s website or the NHS App.
You can choose the way you contact your practice based on what is best for you. Some practices may have longer hours or may ask that you contact them via phone or in person for urgent queries.
What if the practice is closed?
If you need urgent help for your physical or mental health when the general practice is closed, and you cannot wait until they open, go online to 111.nhs.uk or call 111. They will tell you what to do next.
What if it’s an emergency?
If it’s a serious or life-threatening emergency, go straight to A&E (Accident and Emergency) or call 999.
What happens when you contact your practice to request an appointment?
Whether you make your request by phone, on-line or visiting your practice, you may be asked to give your practice some details so that they can assess what is best for you based on your clinical need. The practice team will consider your request for an appointment or medical advice and tell you within one working day what will happen next.
This could be:
- An appointment that day or a subsequent day
- A phone call that day or a subsequent day
- A text message responding to your query
- Advice to go to a pharmacy or another NHS service.
Your practice will decide what is best for you based on your clinical need.
Your practice cannot tell you to just call back the next day.
Who might help you?
You might be offered a face-to-face appointment or a phone call with a GP or other member of the practice staff, like a nurse or pharmacist.
If you have a carer, they can speak for you with your consent.
You can ask to see a preferred healthcare professional, and the practice will try to meet your request, although you might have to wait longer for that person to be available.
It can be helpful to see the same healthcare professional, particularly if you have a long-term health condition.
From what age can you see a GP on your own?
If you are 16 or older, you can make and go to appointments by yourself.
If you are under 16, you can still ask to see a GP without your parent or guardian. The GP will decide if that’s appropriate for you.
What if you need extra help?
If you do not speak English, you can ask for interpretation services in your preferred language when you make an appointment.
If you need extra help like longer appointments, a quiet space, wheelchair access, or information in a different format, tell your practice and they will try to help.
How do you choose a general practice?
You can:
- Call or visit a local practice
- Use Find a GP online.
If you want to change to a new general practice you can do so at any point. Most people have a few choices nearby.
Do you need ID or proof of address?
No, you do not need ID, an NHS number or proof of address. It can help the practice if you do, but it is not needed to register or see a GP. You can also register with a practice if you are homeless.
Can a practice say no to registering you?
They must write to you within 14 days if they say no and explain why. A practice can only say no for a good reason, like if you live too far away or their patient list is closed. For example, they cannot say no for reasons such as immigration status, not having a permanent address, or for reasons connected with other characteristics protected under equalities legislation.
Can you choose which hospital or clinic you are referred to?
If your GP needs to refer you for a physical or mental health condition, in most cases you have the right to choose the hospital or service you’d like to go to. You can get further information on your right to choose on the nhs.uk website.
If you are new to the UK
You can still register with a GP. It’s free to use and your immigration status does not affect your right to register with a GP.
If you are away from home but still in the UK
If you are away from home for more than 24 hours (but less than 3 months), you can register as a temporary patient near where you’re staying.
You can also change your nominated pharmacy so you can get your medicine nearby. You can do this by contacting your practice or via the NHS App.
Do general practices charge for anything?
NHS GP services are free. Sometimes, if you ask the GP to do private work (like writing a letter for insurance), they may charge a fee.
How should everyone be treated?
The practice should treat everyone fairly, kindly and respectfully. Likewise, you should also treat staff with respect. The practice can remove patients from their list if they are violent or abusive to staff.
To learn more about your rights, you can read the NHS Constitution.
How can you help your general practice?
- Be prepared: Before an appointment, think about writing down your symptoms, what you are worried about and what you want to talk about.
- Be on time: Being late for an appointment or being unavailable for a timed call-back can affect other patients.
- Cancel if needed: If you can’t go to your appointment, tell the practice as soon as you can, so that they can offer it to someone else.
- Use the NHS App or website: If you’re confident using smart phones or computers, you can book or cancel appointments, order repeat prescriptions, and see your test results online.
- Turn on notifications: If you use the NHS App, turn on notifications so the practice can contact you more easily. Please keep an eye out for messages.
- Order repeat medicines on time: Make sure you ask for repeat prescriptions on time, so you don’t run out, and only order what you need.
- Join the Patient Participation Group: You practice will have a group of patients who can offer feedback on the services it delivers. Your practice website should explain how you can join.
How can you give feedback or raise concerns?
If you want to give feedback, raise a concern or wish to make a formal complaint, ask to speak to the practice manager. If you don’t feel comfortable doing this, contact your integrated care board (ICB) – the local NHS body that oversees GPs practices. You can find your local integrated care on the NHS England website.
You can also give feedback about your practice to your local Healthwatch. Their job is to make sure NHS leaders and other decision-makers hear your voice and use your feedback to improve care. Healthwatch is independent and impartial, and any information you share with them is confidential. To find your local Healthwatch visit the Healthwatch website.
Privacy Policy
Data Protection Privacy Notice for Patients
Introduction
For the purpose of applicable data protection legislation including the General Data Protection Regulation (EU 2016/679) and the Data Protection Act 2018, the GP practice responsible for your personal data is Rea Valley Health Partnership.
We, Rea Valley Health Partnership, will be known as the ‘Controller’ of the personal data you provide to us.
Your privacy is important to us, and we are committed to protecting and safeguarding your data privacy rights.
This Privacy Notice applies to personal information processed by or on behalf of the Practice. It applies to the personal data of our patients and to the data you have given us about your carers/family members. It covers the following topics:
- Why do we need your data?
- What data do we collect about you?
- What is the legal basis for using your data?
- How do we store your data?
- How do we maintain the confidentiality of your data?
- How long do we keep your data?
- What are your data protection rights?
- Who do we share your data with?
- Are there other projects where your data may be shared?
- When is your consent not required?
- How can you access or change your data?
- What should you do if your personal information changes?
- Changes to our privacy policy
- Our Data Protection Officer
- How to contact the appropriate authorities
Why do we need your data?
As your General Practice, we need to know your personal, sensitive and confidential data in order to provide you with appropriate healthcare services. Your records are used to facilitate the care you receive, and to ensure you receive the best possible healthcare.
Information may be used within the GP practice for clinical audit, to monitor the quality of the service provided.
What data do we collect about you?
Personal data: We collect basic personal data about you which does not include any special types of information or location-based information. This includes your name, postal address and contact details such as email address and telephone number.
By providing the Practice with your contact details, you are agreeing to the Practice using those channels to communicate with you about your healthcare, i.e. by letter (postal address), by voice-mail or voice-message (telephone or mobile number), by text message (mobile number) or by email (email address). If you are unhappy or have a concern about our using any of the above channels, please let us know.
Special Category personal data: We also collect confidential data linked to your healthcare which is known as “special category personal data”, in the form of health information, religious belief (if required in a healthcare context) ethnicity and gender. This is obtained during the services we provide to you and through other health providers or third parties who have provided you with treatment or care, e.g. NHS Trusts, other GP surgeries, Walk-in clinics etc.
Records which the Practice holds about you may include the following information:
- Details about you, such as your address, carer, legal representative, emergency contact details
- Any contact the Practice has had with you, such as appointments, clinic visits, emergency appointments etc.
- Notes and reports about your health
- Details about your treatment and care
- Results of investigations such as laboratory tests, x-rays etc
- Relevant information from other health professionals, relatives or those who care for you
NHS records may be electronic, on paper, or a mixture of both.
Use of CCTV: Closed circuit television is utilised to protect the safety of our patients, staff and members of the public. To maintain privacy and dignity, CCTV is not in place where examinations or procedures are being undertaken. The Practice remains the data controller of this data and any disclosures or requests should be made to the Practice Manager.
What is the legal basis for using your data?
We are committed to protecting your privacy and will only use information collected lawfully in accordance with:
- Data Protection Act 2018
- The General Data Protection Regulations 2016
- Human Rights Act 1998
- Common Law Duty of Confidentiality
- Health and Social Care Act 2012
- NHS Codes of Confidentiality, Information Security and Records Management
Under the General Data Protection Regulation we will lawfully be using your information in accordance with:
Article 6 (e) – “processing is necessary for the performance of a task carried out in the public interest or in the exercise of official authority vested in the controller”
Article 9 (h) – “processing is necessary for the purposes of preventive or occupational medicine, for the assessment of the working capacity of the employee, medical diagnosis, the provision of health or social care or treatment or the management of health or social care systems”
For the processing of special categories data, the basis is:
Article 9 (2) (b) – “processing is necessary for the purposes of carrying out the obligations and exercising specific rights of the controller or of the data subject in the field of employment and social security and social protection law”
These articles apply to the processing of information and the sharing of it with others for specific purposes.
How do we store your data?
We have a Data Protection regime in place to oversee the effective and secure processing of your personal and special category (sensitive, confidential) data. No third parties have access to your personal data unless the law allows them to do so and appropriate safeguards have been put in place.
In certain circumstances you may have the right to withdraw your consent to the processing of data. These circumstances will be explained in subsequent sections of this document.
In some circumstances we may need to store your data after your consent has been withdrawn, in order to comply with a legislative requirement.
How do we maintain the confidentiality of your data?
Our Practice policy is to respect the privacy of our patients, their families and our staff and to maintain compliance with the General Data Protection Regulations (GDPR) and all UK specific Data Protection requirements. Our policy is to ensure all personal data related to our patients will be protected.
We use a combination of working practices and technology to ensure that your information is kept confidential and secure.
Every member of staff who works for an NHS organisation has a legal obligation to keep information about you confidential.
All employees and sub-contractors engaged by our Practice are asked to sign a confidentiality agreement. The Practice will, if required, sign a separate confidentiality agreement if the client deems it necessary. If a sub-contractor acts as a data processor for Sherwood House Medical Practice an appropriate contract will be established for the processing of your information.
Some of this information will be held centrally and used for statistical purposes. Where this happens, we take strict measures to ensure that individual patients cannot be identified.
Sometimes your information may be requested to be used for research purposes. The Practice will always gain your consent before releasing the information for this purpose in an identifiable format. In some circumstances you can Opt-out of the Practice sharing any of your information for research purposes.
How long do we keep your data?
We are required under UK law to keep your information and data for the full retention periods as specified by the NHS Records Management Code of Practice for Health and Social Care and in accordance with National Archives requirements.
More information on records retention can be found online at: Records Management Code of Practice – NHS Transformation Directorate (england.nhs.uk)
What are your data protection rights?
If we already hold your personal data, you have certain rights in relation to it.
Right to object: If we are using your data because we deem it necessary for our legitimate interests to do so, and you do not agree, you have the right to object. We will respond to your request within 30 days (although we may be allowed to extend this period in certain cases). Generally, we will only disagree with you if certain limited conditions apply.
Right to withdraw consent: Where we have obtained your consent to process your personal data for certain activities (for example a research project), or consent to market to you, you may withdraw your consent at any time.
Right to erasure: In certain situations (for example, where we have processed your data unlawfully), you have the right to request us to erase your personal data. We will respond to your request within 30 days (although we may be allowed to extend this period in certain cases) and will only disagree with you if certain limited conditions apply.
Right of data portability: If you wish, you have the right to transfer your data from us to another data controller. We will help with this with a GP to GP data transfer and transfer of your hard copy notes.
National Data Opt-Out: The National Data Opt-Out is a service introduced on 25 May 2018 that allows people to opt out of their confidential patient information being used for research and planning purposes. The National Data Opt-Out replaces the previous Type 2 Opt-Out, which required NHS England not to share a patient’s confidential patient information for purposes beyond their individual care. Any patient who had a Type 2 Opt-Out has had it automatically converted to a National Data Opt-Out from 25 May 2018 and has received a letter giving them more information and a leaflet explaining the new service. If a patient wants to change their choice, they can use the new service to do this. You can find out more from the Practice or by visiting:
https://www.nhs.uk/your-nhs-data-matters/
If you wish to raise a query or request relating to any of the above, please contact us. We will seek to deal with it without undue delay, and in any event in accordance with the requirements of any applicable laws. Please note that we may keep a record of your communications to help us resolve any issues which you raise.
Who do we share your data with?
We consider patient consent as being the key factor in dealing with your health information.
To provide around-the-clock safe care, we will make information available to trusted organisations for specific purposes unless you have asked us not to. We refer to these organisations to Data Processors.
To support your care and improve the sharing of relevant information to our partner organisations when they are involved in looking after you, we will share information to other systems. The general principle is that information is passed to these systems unless you request that this does not happen, but that system users should ask for your consent before viewing your record.
Our partner organisations are:
- NHS Trusts / Foundation Trusts
- GPs
- NHS Commissioning Support Units
- Independent Contractors such as dentists, opticians, pharmacists
- Private Sector Providers
- Voluntary Sector Providers
- Ambulance Trusts
- Integrated Commissioning Board (ICB)
- Social Care Services
- NHS England (NHSE) and NHS Digital (NHSD)
- Multi Agency Safeguarding Hub (MASH)
- Local Authorities
- Education Services
- Fire and Rescue Services
- Police and Judicial Services
- Voluntary Sector Providers
- Private Sector Providers
- Other ‘data processors’ which you will be informed of
You will be informed who your data will be shared with, and in cases where your consent is required you will be asked for it.
Below are some examples of when we would wish to share your information with trusted partners.
Primary Care Networks: We have formed a Primary Care Network. This means we work closely with a number of local practices and care organisations for the purpose of direct patient care. They will only be allowed to access your information if it is to support your healthcare needs. If you have any concerns about how your information may be accessed within our primary care network, we would encourage you to speak or write to us.
Extended Access: We provide extended access services to our patients which means you can access medical services outside of our normal working hours. In order to provide you with this service, we have formal arrangements in place with the Clinical Commissioning Group and with other practices whereby certain key “hub” practices offer this service on our behalf for you as a patient to access outside our opening hours. Those key “hub” practices will need to have access to your medical record to be able to offer you the service. We have robust data sharing agreements and other clear arrangements in place to ensure your data is always protected and used for those purposes only.
Medicines Management: The Practice may conduct Medicines Management Reviews of medications prescribed to its patients. This service performs a review of prescribed medications to ensure patients receive the most appropriate, up-to-date and cost-effective treatments. Our local NHS ICB employs specialist pharmacists and they may at times need to access your records to support and assist us with prescribing. This reason for this is to help us manage your care and treatment.
Individual Funding Requests: An Individual Funding Request is a request made on your behalf, with your consent, by a clinician, for the funding of specialised healthcare which falls outside the range of services and treatments that the ICB has agreed to commission for the local population. An Individual Funding Request is considered when a case can be set out by a patient’s clinician that there are exceptional clinical circumstances which make the patient’s case different from other patients with the same condition who are at the same stage of their disease, or when the request is for a treatment that is regarded as new or experimental and where there are no other similar patients who would benefit from this treatment. A detailed response, including the criteria considered in arriving at the decision, will be provided to the patient’s clinician.
Are there other projects where your data may be shared?
Local Research: We regularly work with local health and academic organisations to conduct research studies with the aim of improving care for the general population. We will always ask for your permission to take part, except in situations where we can demonstrate that your information has been anonymised (where you cannot be identified) and your privacy is protected. In these situations we are not required to seek consent from individuals.
Risk Stratification: Risk stratification data tools are increasingly being used in the NHS to help determine a person’s risk of suffering a condition, preventing an unplanned admission or re-admission and identifying a need for preventive intervention. Information about you is collected from a number of sources including NHS Trusts and from this GP practice. A risk score arrived at through an analysis of your de-identified information is provided back to your GP practice as data controller in an identifiable form. Risk stratification enables your GP to focus on preventing ill health and not just the treatment of sickness. If necessary, your GP may be able to offer you additional services. Please note that you have the right to opt out of your data being used in this way.
Other research projects: With your consent we would also like to use your name, contact details and email address to inform you of services that may benefit you. There may be occasions when authorised research facilities would like to invite you to participate in research, innovations, identifying trends or improving services. At any stage where we would like to use your data for anything other than the specified purposes and where there is no lawful requirement for us to share or process your data, we will ensure that you have the ability to consent or to opt out prior to any data processing taking place. This information is not shared with third parties or used for any marketing and you can unsubscribe at any time via phone, email or by informing the Practice.
OpenSAFELY: “NHS England has been directed by the government to establish and operate the OpenSAFELY COVID-19 Service and the OpenSAFELY Data Analytics Service. These services provide a secure environment that supports research, clinical audit, service evaluation and health surveillance for COVID-19 and other purposes.
Each GP practice remains the controller of its own GP patient data but is required to let approved users run queries on pseudonymised patient data. This means identifiers are removed and replaced with a pseudonym.
Only approved users are allowed to run these queries, and they will not be able to access information that directly or indirectly identifies individuals.
Patients who do not wish for their data to be used as part of this process can register a type 1 opt out with their GP.
When is your consent not required?
We will only ever use or pass on information about you to others involved in your care if they have a genuine need for it. We will not disclose your information to any third party without your permission unless there are exceptional circumstances.
There are certain circumstances where we are required by law to disclose information, for example:
- where there is a serious risk of harm or abuse to you or other people
- where a serious crime, such as assault, is being investigated or where it could be prevented
- notification of new births
- where we encounter infectious diseases that may endanger the safety of others, such as meningitis or measles (but not HIV/AIDS)
- where a formal court order has been issued
- where there is a legal requirement, for example if you had committed a Road Traffic Offence
We are also required to act in accordance with Principle 7 of the Caldicott Review (Revised version 2013) which states: “The duty to share information can be as important as the duty to protect patient confidentiality.” This means that health and social care professionals should have the confidence to share information in the best interests of their patients within the framework set out by the Caldicott Principles.
How can you access or change your data?
You have a right under the Data Protection legislation to request access to view or to obtain copies of the information the Practice holds about you and to have it amended should it be inaccurate.
Your request should be made to the Practice and we have a form (SAR – Subject Access Request) which you will need to complete. We are required to respond to you within one calendar month.
For information from the hospital you should write direct to them. You will need to give adequate information (full name, address, date of birth, NHS number and details of your request) so that your identity can be verified and your records located.
There is no charge to receive a copy of the information held about you.
What should you do if your personal information changes?
Please contact the Practice Manager as soon as any of your details change. This is especially important for changes of address or contact details (such as your mobile phone number).
The Practice will from time to time ask you to confirm that the information we currently hold is accurate and up-to-date.
Changes to our privacy policy
It is important to point out that we may amend this Privacy Notice from time to time.
Our Data Protection Officer
The Practice has appointed Umar Sabat as its Data Protection Officer.
He can be contacted on the following e-mail address: umar.sabat@ig-health.co.uk
If you have any concerns about how your data is shared, or if you would like to know more about your rights in respect of the personal data we hold about you, then please contact the Practice Data Protection Officer.
How to contact the appropriate authorities
If you have any concerns about how your information is managed at your GP Practice, please contact the GP Practice Manager or the Data Protection Officer in the first instance.
If you are still unhappy following a review by the GP Practice, you have a right to lodge a complaint with the UK supervisory authority, the Information Commissioner’s Office (ICO), at the following address:
Information Commissioner
Wycliffe House
Water Lane
Wilmslow
Cheshire
SK9 5AF
Tel: 01625 545745
Email: https://ico.org.uk/
Shared Care Prescribing Policy
This document is based on Principles for Shared Care Prescribing as per the BMA which was updated on 28th April 2025. See link: Prescribing in general practice.
Shared Care Prescribing refers to medication which is initiated by a specialist and ongoing prescribing and monitoring is shared with a GP practice, usually accompanied by guidance or a shared care agreement.
The GMC has guidance on shared care prescribing which requires a clinician to be informed about the side effects of the medication and undertake the required monitoring.
The following principles should apply to all shared care prescribing.
- Shared care prescribing is non-core voluntary activity that can be declined by the GP practice for any of the reasons stated below:
This includes:
– Inadequate capacity within the practice
– Inadequate competency about the specialist medication, despite training
– Lack of assurance to provide the ongoing specialist support required for shared care.The practice will ensure any refusal is consistent and framed by a set of principles so it is not discriminatory to specific patient groups or individual patients.
- The GP practice is satisfied with the quality assurance and clinical governance of the specialist provider
- If ongoing medical monitoring is required, responsibility for this should be clear within associated guidance in the form of a shared care agreement
- The appropriate stabilisation period has occurred before prescribing is handed over to the GP practice and it is clear that should the patient require specialist support that the patient will be consulted and re-referred to a Specialist. a. The duration is determined by the shared care agreement (often 3 months).
- There is enduring specialist input
For example:
– Ongoing out-patient follow-up
– A mechanism which allows timely advice from the specialist, which could be converted into an out-patient review.
Roles and Responsibilities of parties involved
- Specialist Responsibilities:
- Initiate treatment and stabilise the patient on the medication.
- Provide the GP with comprehensive information about the patient’s condition, treatment plan, and any monitoring requirements.
- Ensure the patient understands the shared care arrangement and consents to it.
- Remain available for consultation and advice as needed.
- GP Responsibilities:
- Assess whether they have the necessary expertise and resources to take on shared care responsibilities.
- Prescribe the medication as per the specialist’s guidance once the patient is stabilized.
- Monitor the patient’s progress and report any concerns to the specialist.
- Ensure the patient understands their treatment and any necessary follow-up.
- Patient Responsibilities:
- Attend all appointments and follow the treatment plan as advised.
- Report any side effects or concerns to their GP or specialist promptly.
- Understand the shared care arrangement and their role within it.
Communication
- A formal written agreement/protocol should be established, detailing the responsibilities of each party.
- Regular communication between the GP and specialist is essential to ensure continuity of care.
- Any changes in the patient’s condition or treatment plan should be communicated promptly.
Review
This document will be reviewed on an annual basis or amended based on BMA changes.
Summary Care Record
There is a new Central NHS Computer System called the Summary Care Record (SCR). It is an electronic record which contains information about the medicines you take, allergies you suffer from and any bad reactions to medicines you have had.
Why do I need a Summary Care Record?
Storing information in one place makes it easier for healthcare staff to treat you in an emergency, or when your GP practice is closed.
This information could make a difference to how a doctor decides to care for you, for example which medicines they choose to prescribe for you.
Who can see it?
Only healthcare staff involved in your care can see your Summary Care Record.
How do I know if I have one?
Over half of the population of England now have a Summary Care Record. You can find out whether Summary Care Records have come to your area by looking at our interactive map or by asking your GP
Do I have to have one?
No, it is not compulsory. If you choose to opt out of the scheme, then you will need to complete a form and bring it along to the surgery. You can use the form at the foot of this page.
More Information
For further information visit the NHS Care records website
Violence Policy
The NHS operate a zero tolerance policy with regard to violence and abuse and the practice has the right to remove violent patients from the list with immediate effect in order to safeguard practice staff, patients and other persons.
Violence in this context includes actual or threatened physical violence or verbal abuse which leads to fear for a person’s safety.
In this situation we will notify the patient in writing of their removal from the list and record in the patient’s medical records the fact of the removal and the circumstances leading to it.
